Some people are bothered that I can do all these things. Some want to know why I have managed to live a normal life for so long when other people with dementia seem to deteriorate so fast. Some even think I’m faking it – that there is, in fact, nothing wrong with me. I fake it every day. I fake being a “normal” person.
Every single day is a struggle for me and occasionally I take to my bed. Sometimes for hours, sometimes for days, just from the exhaustion of travelling, smiling, talking, thinking and responding.
When I speak, most of my sentences do not have the words or grammar I seek for them and I speak much slower than I once did. I feel constantly disappointed with myself and worry all the time that I will get lost in the middle of a sentence.
If you were to speak to me for a short amount of time you would notice none of this. I may not dazzle you with my vocabulary or remember what I had for breakfast, but I can converse quite well if I take it slow and relax, and have plenty of rest before and after we meet.
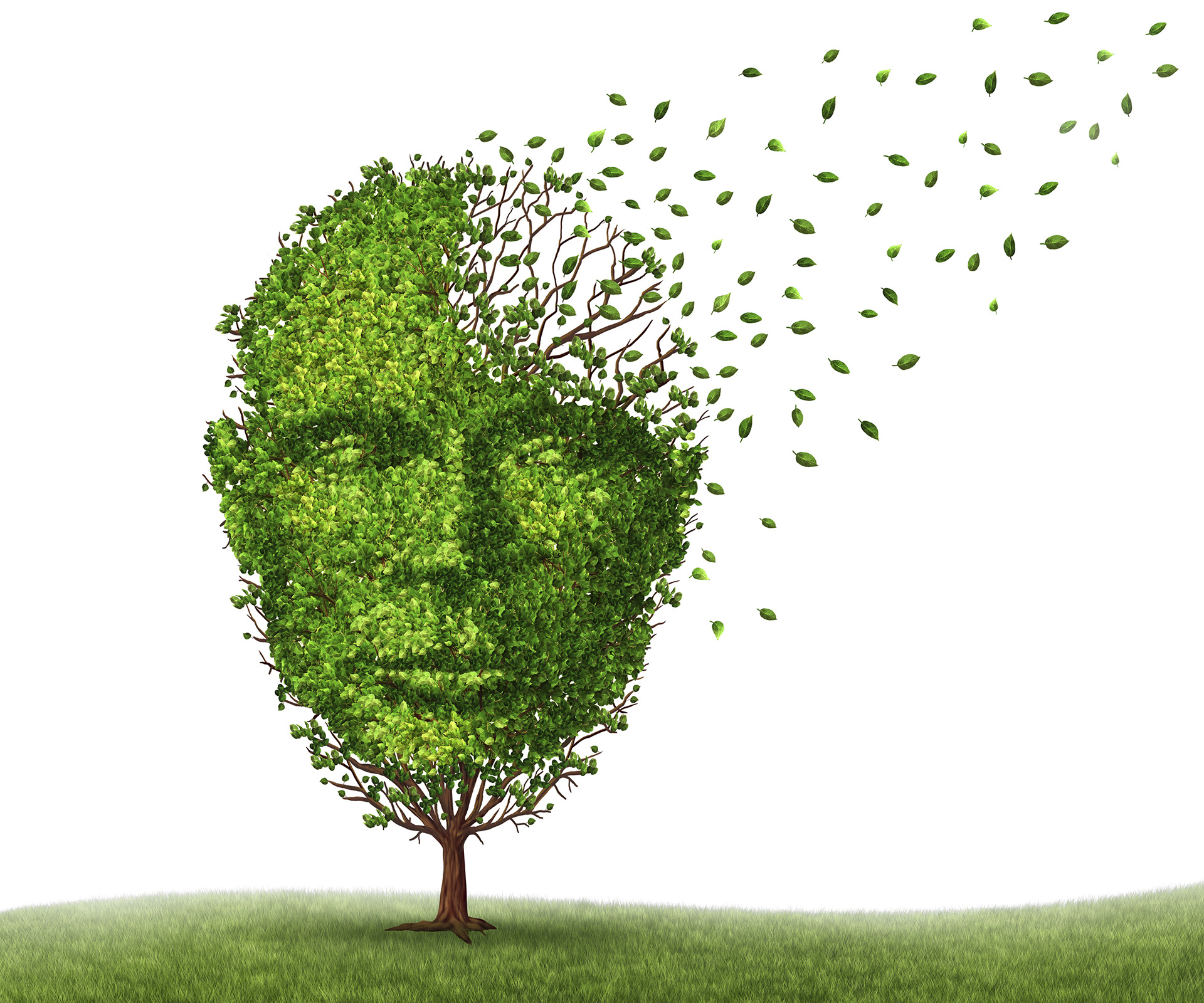
Dementia itself is not a disease, but a way of describing a progressive decline in memory or other thinking skills.
Alzheimer’s disease is the most common cause of dementia. There are three things to say about my dementia upfront: firstly, there is no doubt as to my diagnosis. There has been a progressive, measurable atrophy (wasting away) of my brain tissue over the past 20 years, shown on CT, PET and MRI scans, and my performance on neuropsychological tests has shown a decline as well. Secondly, my form of dementia is unusual because it is progressing very slowly – much slower than average – and despite numerous tests the experts are unable to pinpoint the exact cause of it. Nobody will know for sure what form of dementia I have until they are able to biopsy my brain – and I need every brain cell I have right now, so that moment of truth won’t happen until after I die. And thirdly, before my dementia, my brain was functioning at a very high level – possibly in the top couple of percentiles in the world – so in order to understand how much I’ve lost, you need to understand how much I once had.
Before and After
There’s a clear dichotomy to my adult life and it is divided by the moment a doctor told me I had dementia. Before that day, I was a whip-smart, multitasking scientist on a clear career trajectory that seemed sky-high. I was also a dedicated mother, aware of all that was going on in my children’s lives, spending all my spare time with them, talking, reading, sitting with them. As soon as I was told that my brain had a degenerative, incurable disease, I felt exiled from my former self and life.
It was 1995. My divorce had just been finalised. My two youngest daughters (then aged 14 and nine) and I had spent the weekend moving into our new home – a house in Canberra we had just bought.
My eldest daughter (aged 20) was in Sydney at university. I held a senior job in the public service: I was the first assistant secretary in the Department of the Prime Minister and Cabinet, heading up a division and advising the Prime Minister on science and technology.
But for the previous year or so something hadn’t been right. I was having trouble coping at work. A few things were slipping through my hitherto vice-like brain and I was suffering from crippling migraines that would last for days, sometimes occurring up to once a week.
And that is how I came to be sitting in a neurologist’s surgery on a bright, clear Canberra Monday morning, on 22 May, 1995.
“Yes, it’s definitely Alzheimer’s,” he said. I thought I’d misheard him. “How long … do I have?” I asked.
“Early-onset Alzheimer’s typically advances very quickly,” he said. “Usually from diagnosis there are five years until the patient needs care with basic needs, then another two or three years in a nursing home until they die.”
I still remember the devastation of that initial diagnosis, the year of follow-up testing with another, more sympathetic neurologist, and my desperate hope that there had been some mistake. And overriding all of this was the feeling that I had nothing further to offer society or my own children and how worthless and incapable and alone I was.
There’s no cure for dementia and I haven’t been cured. A cursory look at my scans would tell any competent doctor that my brain isn’t what it should be. But what I didn’t realise at the time was how much I still had to offer the world. I was to show people all over the world, people with dementia and people who love them and people who work with them, that a diagnosis of dementia doesn’t necessarily equate to a worthless life. You can live a rich life with dementia. And I’ve even been able to re-wire the healthy portion of my brain to make the most of what I’ve got left.

Left to right: Christine receiving the public service medal for outstanding service to science and technology in the Queen’s Birthday Honours in 1994; accepting her diploma; out in the field during her work.
A New Career
In 1980, there were two big changes to my life. I didn’t want another child, so I was taking the contraceptive pill.
[My then husband] had asked me to stop taking it; he wanted to try for a boy. I hadn’t yet stopped, but nonetheless in 1980, I fell pregnant.
The other big change was that my friend Judy, who worked at the CSIRO (Commonwealth Scientific and Industrial Research Organisation), told me about a job that was being advertised – the job of scientific information officer.
The position was based in Sydney and involved research and writing about the minerals and energy section of the organisation.
I often say that starting work at the CSIRO was like coming home. Apart from the births of my daughters, this was the one big part of my life that felt like it had been missing. For so many years, my poor brain had been cut adrift from scientific research and now at last its blindfold would be removed so that it could begin to flourish and grow once more.
The Courage to Leave
Looking back at that time, in my late 30s, I can see one of the very earliest signs that all was not well with my brain. I had to travel regularly by car between laboratories in North Ryde and Lucas Heights, Sydney, and also to the head office in Canberra.
At the beginning, this was a breeze, but after a year or so, I’d reach the gate of our own laboratory complex and try to recall which way to turn for the trip I was about to make. And, one day, I recall stopping by the side of the road in the middle of Sydney, totally confused about how to proceed to get to Lucas Heights. Of course, the last thing I ever thought of was dementia back then.
Then, in 1989, I was invited to apply for the job of first assistant secretary in the Department of the Prime Minister and Cabinet, heading up the office of the chief scientist.
I loved my new job. I felt like a learning machine – learning in order to impart to others new possibilities and dreaming of new futures. My mind was buzzing with ideas, lateral concepts and challenges. I worked during the consecutive governments of Bob Hawke and Paul Keating, and it was a thrilling time.
In May 1993, I piled up the car with Ianthe (aged 18), Rhiannon (12), Micheline (seven), our old cat, Buzz (16), and even our two budgies. We pulled out of the driveway as a removal van with our share of the house pulled away from the kerb, heading to our new home.
What lay ahead
One evening, I had to drive Ianthe to her evening maths tutoring job, a trip I’d done quite a few times before, but she still had to say left, right, straight ahead on the way out there. But on the return trip, as we started off for home, she naturally assumed I’d be able to find my way back. But I felt very lost – everything looked so different going the other way.
I felt flustered. “I’ve got a lot on my mind,” I snapped. “Just tell me the way to get home. I can’t remember.” She must have been very puzzled as to why I could not find my way home, when we had only an hour or so ago done the same journey in reverse. But, of course, neither of us had any idea that the mapping system in my brain had disappeared.
My brain map had even disappeared when it came to working out the very familiar route to the girls’ schools and then on to work. It was okay when I made a few mistakes after dropping them off, but they were very alarmed when I would make a wrong turn with all of them piled into the car. One time, it happened when I was only just at the end of our street.
At work, I was relying more and more on my personal assistant, Margaret, who developed a very detailed daily work schedule for me. Each minute of my day was laid out. I still have a copy of the last one I was using when I finally left work – it lists meetings, people, places, all allocated to very tight time slots.
(Now I have no recollection even of those very important meetings I was chairing. What do those acronyms mean? I must have once known what they all were.) And she’d come and get me out of a meeting when it was time for me to go to the next one, as she realised I would forget otherwise. Not only did she keep me on track at work, but she’d also remember my poor girls, who’d have to be collected from after-school care, or taken to my office to wait for me after a late meeting.

A Dark Day with Dementia
I want to talk about what my worst day looks like. Not every day is like this, but elements of this struggle do colour my every day. Some mornings when I wake up, I have no idea what day it is or what we are meant to be doing. Am I going out? Is someone coming to visit? I can’t put today in context by remembering what day of the week or month it is, or by remembering yesterday – yesterday is a black hole for me, too. Already, just lying in bed, I feel adrift and at a loss.
I have no frame of reference for my day. Some afternoons, I feel quite sharp, my memories of the day clear; I can remember what happened that morning. But there are days when each memory slips away, as though I have lost all but one remaining key to the filing cabinet of my memories. Did I just take my tablet? Do I have a doctor’s appointment today? I feel as if I am hanging onto a cliff above a deep, dark, stormy sea of unknowing.
Writing anything by hand is now something I rarely do. The letters often look peculiarly shaped and the odd one is missing, and they do not come out in the right order. So I feel happier trying to tap out things on the computer where there is a spell check to help me.
Ironing can be hazardous. I have to concentrate very hard to make sure that I know where these body parts of mine are and that they are out of harm’s way. Emptying the dishwasher is like doing a real brain test of working out where things belong, when there are so many different items.
On a bad day, when I’m at home alone, I might pace around, making cups of tea, starting the washing or some other activity, but then forgetting what I’m in the middle of doing. The washing might sit in the machine – even though it beeps when it finishes, if I don’t hang it out immediately and become involved in other activities, I’ll completely forget about it. So my day can be spent rushing around in a disjointed way doing disconnected things. And as I remember something to do, I rush to write it on the board or in my iPhone, muttering to myself as I walk hurriedly to the kitchen.
If I do not talk aloud to myself, the thought will disappear, so that by the time I get to the board or phone, I have no idea why I am there.
Testing Times
Things were hard for us. There wasn’t the support for people with dementia that there is now, nor any support at all for young children whose lives have been affected by a family member having the condition. Around this time, I looked up Alzheimer’s Australia in the phone book and called them.
“I’d like to talk to someone about getting support for our family,” I said.
“Of course,” said a sympathetic voice on the phone. “And who are you caring for? Your husband? Or a parent?”
“I’m not a carer,” I said. “I have Alzheimer’s.” That floored her.
“Oh,” she said. “Oh, well we have lots of information I can send your carer …” That conversation sticks out in my mind as one of the first moments that thought, “That’s not right. Why on earth is there support for the carer and not the person who actually has dementia?” This outrage was the first seed planted in what was to become my resolution to be an advocate for people with dementia.
Hanging In There
I do think that my attitude to life and to dementia has helped me a lot. I choose to try to live positively. In so doing, I am making a journey into the centre of self, away from the complex cognitive outer layer that once defined me, through the jumble and tangle of emotions created through my life experiences, into the centre of my being, into what gives me true meaning in life.
This, I hope, will remain intact despite the ravages of dementia.
I have chosen to be a dementia survivor, living life positively each day, with my enabler, Paul, alongside me.
My attitude to life is positive – I am charging out of the trenches of despair, waving my tattered flag of effort and rehab. I will be bold. I will seize the moment. I will even try to excel.
There’s a drama to this survival, of hanging on and yet aiming high. I am celebrating my 20-year survival, looking back over the roller-coaster ride it took to get there.
And I intend to last as long as possible. When I look at what might lie ahead for me, it is this that drives me even more each day to keep striving. I’m in my last battle to survive – to live as best I can, while I can.

This is an edited extract from Before I Forget: How I survived a Diagnosis of Younger-Onset Dementia at 46 by Christine Bryden, published by Viking. Also available as an eBook. A version of this extract originally appeared in The Australian Women’s Weekly’s Summer Health 2015 issue.
VIDEO: A grieving mother listens to her late son’s heartbeat 3 years after his death